RADAR: Detecting Childhood Cancer Treatment Dropouts Before They Happen
By Antonella Ardila, GRC 2024 Global Essay Competition Top 30
“Every child with cancer deserves a chance at survival, and that begins with ensuring they receive the full course of treatment” (Grillo 2024). Unfortunately, treatment abandonment remains a significant challenge in pediatric oncology, especially in Latin American countries like Colombia. The cumulative incidence of treatment abandonment in Colombia is 9% at 24 months and survival probability in children who abandon treatment significantly decreases to 20% in 40 months, while children who continue treatment expect a 67% survival probability in the same time span (VIGICANCER cohort, 2015-2021). That is why it's imperative to address this issue, and develop a preventative healthcare strategy that mitigates treatment abandonment risk.
The development of RADAR, a treatment abandonment risk score developed by Dr. Elvia Karina Grillo, can help tackle the situation and prevent possible treatment abandonment episodes, with a 70% probability of distinguishing between treatment abandonment cases and non treatment abandonment events.
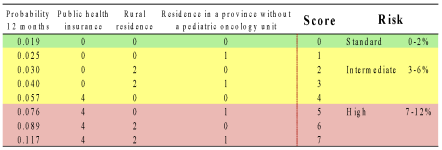
This score was developed using data from children under 15, registered in the childhood cancer surveillance system (named VIGICANCER) database from 2009-2020, in 10 Colombian cities (Bogotá, Bucaramanga, Cartagena, Cali, Ibagué, Neiva, Manizales, Medellín, Monteria & Pasto). RADAR analyzed different predictive variables that might influence the treatment abandonment risk in patients, including rural residence, insurance type and residence in a territory without an oncology center. These three variables were examined in patients, and points were assigned accordingly by RADAR. If the patient’s insurance was public, they would earn 4 points, if the patient lived in a rural area, they were assigned 2 points and if they resided in a territory without an oncology center, they would get 1 point.(There were no points if the patient had private insurance, lived in an urban area, or had easy access to an oncology center).
Figure 1 organizes individuals into three categories based on their overall score. Patients scoring 0 (reflecting favorable conditions, such as being part of a solid affiliation regime and living in a more urbanized area) are classified into the standard risk group (represented in green), which corresponds to the lowest probability of treatment abandonment (0-2% chance of abandoning treatment). Scores ranging from 1 to 4 (highlighted in yellow) indicate the presence of certain risk factors, and a moderate probability of treatment abandonment (3-6% chance of abandoning treatment) while, individuals in the red section, with scores ranging from 5 to 7 (indicating significant risk factors) have the highest likelihood of abandoning treatment (7-12% chance.)
Figure 1:
To minimize these risks, RADAR employs appropriate medical interventions and psychological support to diminish the likelihood of treatment abandonment across all risk categories. As soon as a score is generated, doctors are informed of the patient's risk level. This triggers a thorough analysis of the patient and alongside the psychologist, interventions (such as talks emphasizing the importance of continuing treatment) are made, as well as notes and referrals to highlight the patient’s risk and ensure targeted follow-up actions.
To further validate its efficiency, RADAR was presented to a panel of experts from various oncology treatment centers in Cali. The multidisciplinary team consisted of five pediatric oncohematologists, one pediatrician, three nurses specialized in oncology nursing, a nurse coordinator from an oncohematology service, a social worker, a psychologist, and an advocacy representative from a foundation, who analyzed the risk score and determined its efficiency as a preventive healthcare strategy.
While the current results represent a significant achievement, future versions aim to enhance its predictive capacity by incorporating new predictors and adapting to various international contexts, thus aiming to integrate this risk score worldwide. By doing so, positioning RADAR as a valuable tool in clinical settings, helping to prevent childhood cancer treatment abandonment and improve patient outcomes.
Bibliography:
Abstracts - Pediatric Blood & Cancer. November 2, 2023. https://onlinelibrary.wiley.com/doi/full/10.1002/pbc.30748. EP604/#1102.
Atun R, Bhakta N, Denburg A, Frazier AL, Friedrich P, Gupta S, et al. 2020. "Lancet Oncology Commission on sustainable care for children with cancer." Lancet Oncol. 21(4):e185–224.
Elvia Grillo, Jesús Ardila, Luis Eduardo Bravo, Óscar Ramírez. “RADAR_GrilloVF.pdf,” n.d. https://drive.google.com/file/d/18QpiM7g1tmzFr6siH-Dy2zLanUWtVi5r/view.
Elvia Grillo. “SIOP-2023_PPT_RADAR,” n.d. https://drive.google.com/file/d/1i1DAJ71dKBTIh_NpHc5KIjq6sCvkKGOZ/view.
Friedrich, Paola, Catherine G. Lam, Elena Itriago, Rafael Perez, Raul C. Ribeiro, and Ramandeep S. Arora. “Magnitude of Treatment Abandonment in Childhood Cancer.” PLoS ONE 10, no. 9 (September 30, 2015): e0135230.https://doi.org/10.1371/journal.pone.0135230.
Fundación POHEMA. “Vigicáncer Estudio Encargado De Identificar Los Factores Asociados Al Cáncer Infantil,” October 9, 2024. https://pohema.org/vigicancer/.
Ramirez, Oscar, Paula Aristizabal, Alia Zaidi, Anne Gagnepain-Lacheteau, Raul C. Ribeiro, and Luis E. Bravo. 2018. “Childhood Cancer Survival Disparities in a Universalized Health System in Cali, Colombia.” Pediatric Hematology Oncology Journal 3 (4): 79–87. https://doi.org/10.1016/j.phoj.2019.01.001.
SIOP 2023 - Annual Congress of the International Society of Paediatric Oncology. “SIOP 2023 (International Paediatric Oncology Congress).” SIOP 2023, November 21, 2023. https://2023.siop-congress.org/.
Universidad del Valle. “Cáncer Infantil,” n.d. http://rpcc.univalle.edu.co/index.php/infantil.
Universidad del Valle. “Home.” Facultad de Salud / Universidad del Valle / Cali, Colombia. n.d. https://salud.univalle.edu.co/.
Universidad del Valle. “Radar: Una Alarma Temprana Para El Abandono Del Tratamiento Del Cáncer En Niños,” December 4, 2023.




